大气细颗粒物(PM2.5)在全球范围内每年造成约414万人早逝,其中因动脉粥样硬化性心血管疾病早逝者占50%以上。然而,目前对于PM2.5影响动脉粥样硬化性心血管疾病的分子机制的认识还十分有限。鞘脂是一类脂质生物调控分子,毒理学研究表明其通过影响机体内含载脂蛋白B脂蛋白的水平促进动脉粥样硬化风险。然而,在人群研究层面目前缺乏鞘脂在PM2.5影响动脉粥样硬化中作用的证据。
2013至2015年,12BET注册朱彤教授团队和12BET医院进行合作,完成了对120名受试者共计589人次的健康随访。本研究基于团队自主研发的快速、高通量靶向鞘脂组学分析技术,对受试者血浆中神经酰胺、鞘磷脂、己糖神经酰胺、乳糖神经酰胺等多种鞘脂进行了准确定量测量,发现了大气污染影响动脉粥样硬化的潜在分子机制。
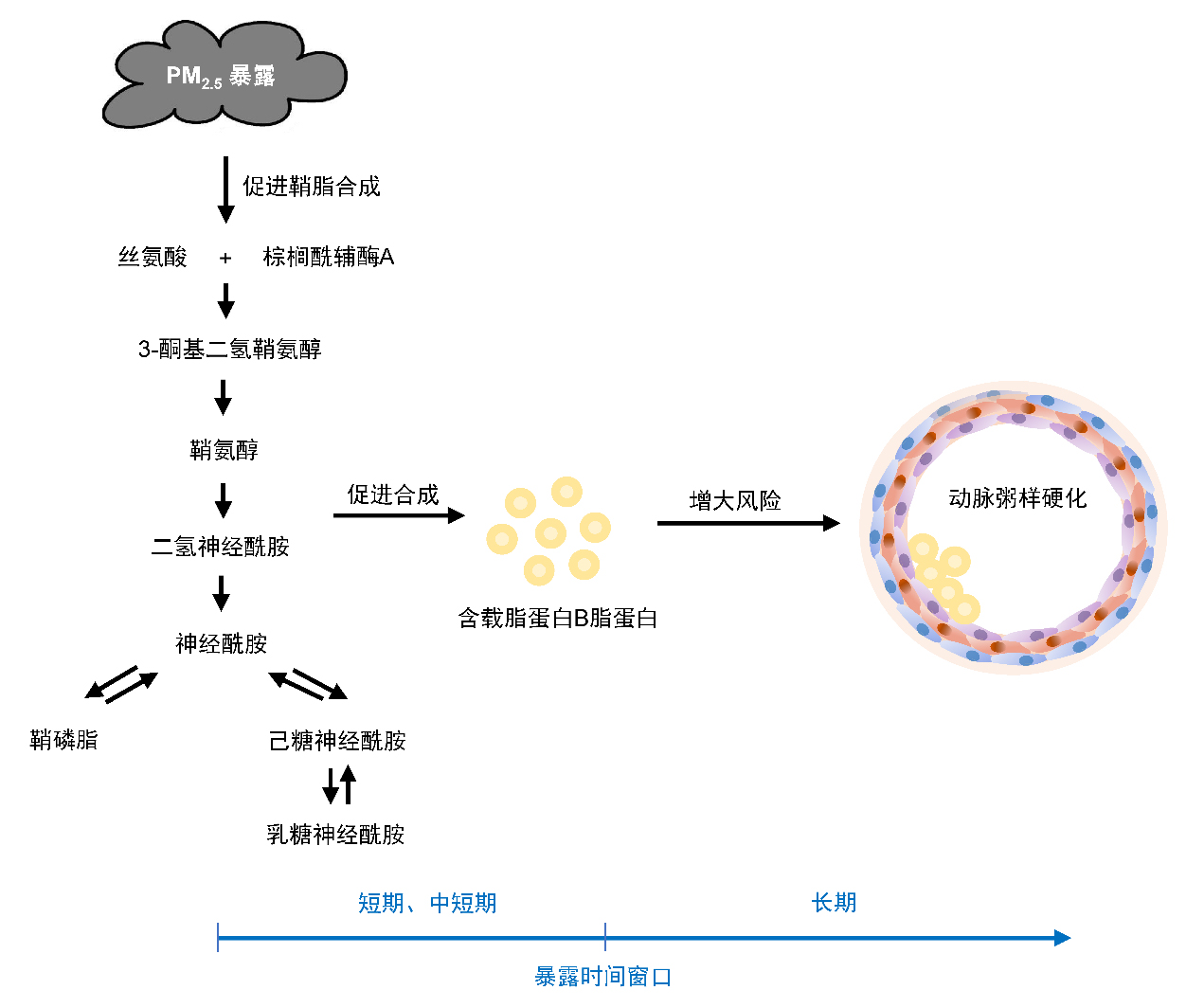
研究发现,PM2.5短期和中短期暴露可能促进人体鞘脂合成(表现为侧链含16至24个碳原子的神经酰胺、鞘磷脂、己糖神经酰胺和乳糖神经酰胺水平的升高),其进一步介导了体内含载脂蛋白B脂蛋白水平的升高。该研究表明鞘脂可能是PM2.5影响动脉粥样硬化性心血管疾病的早期机制,提示基于鞘脂代谢的干预或许会降低空气污染的心血管健康影响。
美国心脏协会心血管著名期刊Arteriosclerosis, Thrombosis, and Vascular Biology于2022年6月2日在线发表了朱彤团队的这一研究成果“Ambient Air Pollution and Atherosclerosis: A Potential Mediating Role of Sphingolipids”。12BET注册的博士生徐一凡、及现为英国帝国理工博士后韩逸群为该论文共同第一作者,朱彤为通讯作者。该项研究获得国家自然科学基金(21190051、91844000、41421064、41121004)和科技部973项目(2015CB553401)的支持,并获得北京老员工物医学伦理委员会的批准(IRB0000105213024)。
论文信息及链接:
Xu Y, Han Y, Wang Y, et al. Ambient Air Pollution and Atherosclerosis: A Potential Mediating Role of Sphingolipids. Arteriosclerosis, Thrombosis, and Vascular Biology, 2022; 42(7): 906-918.
https://doi.org/10.1161/ATVBAHA.122.317753
SCOPE项目相关文章:
Xu Y, Li H, Han Y, et al. A simple and rapid method for extraction and measurement of circulating sphingolipids using LC–MS/MS: a targeted lipidomic analysis. Analytical and Bioanalytical Chemistry, 2022; 414(6): 2041-2054.
https://doi.org/10.1007/s00216-021-03853-z
Chen W, Han Y, Wang Y, et al. Glucose metabolic disorders enhance vascular dysfunction triggered by particulate air pollution: A panel study. Hypertension, 2022;79(5):1079-1090.
https://doi.org/10.1161/HYPERTENSIONAHA.121.18889
Jiang X, Han Y, Qiu X, et al. Personal exposure to electrophilic compounds of fine particulate matter and the inflammatory response: The role of atmospheric transformation. Journal of Hazardous Materials. 2022;432:128559.
https://doi.org/10.1016/j.jhazmat.2022.128559
Lin Y, Zhang H, Han Y, et al. Field evaluation of a potential exposure biomarker of methylated polycyclic aromatic hydrocarbons: Association between urinary phenanthrene-2-carboxylic acid and personal exposure to 2-methylphenanthrene. Environmental Science & Technology Letters. 2022;9(2):166-172.
https://doi.org/10.1021/acs.estlett.1c00938
Wang T, Han Y, Li H, et al. Fine particulate matter and vasoactive 20-hydroxyeicosatetraenoic acid: Insights into the mechanisms of the prohypertensive effects of particulate air pollution. Science of The Total Environment. 2022;806(3):151298.
https://doi.org/10.1016/j.scitotenv.2021.151298
Shi Y, Han Y, Wang Y, et al. Serum branched-chain amino acids modifies the associations between air pollutants and insulin resistance. Ecotoxicology and Environmental Safety. 2021;225:112780.
https://doi.org/10.1016/j.ecoenv.2021.112780
Wang T, Han Y, Li H, et al. Proinflammatory lipid signals trigger the health effects of air pollution in individuals with prediabetes. Environmental Pollution, 2021;290:118008.
https://doi.org/10.1016/j.envpol.2021.118008
Jiang X, Han Y, Qiu X, et al. Organic components of personal PM2.5 exposure associated with inflammation: Evidence from an untargeted exposomic approach. Environmental Science & Technology. 2021;55(15):10589-10596.
https://doi.org/10.1021/acs.est.1c02023
Wang T, Han Y, Li H, et al. Changes in bioactive lipid mediators in response to short-term exposure to ambient air particulate matter: A targeted lipidomic analysis of oxylipin signaling pathways. Environmental International, 2021;147:106314.
https://doi.org/10.1016/j.envint.2020.106314
Chen W, Han Y, Wang Y, et al. Associations between changes in adipokines and exposure to fine and ultrafine particulate matter in ambient air in Beijing residents with and without pre-diabetes. BMJ Open Diabetes Research and Care, 2020;8:e001215.
https://doi.org/10.1136/bmjdrc-2020-001215
Fan Y, Han Y, Liu Y, et al. Biases arising from the use of ambient measurements to represent personal exposure in evaluating inflammatory responses to fine particulate matter: Evidence from a panel study in Beijing, China. Environmental Science & Technology Letters, 2020;7(10):746-752.
https://doi.org/10.1021/acs.estlett.0c00478
Chen X, Han Y, Chen W, et al. Respiratory inflammation and short-term ambient air pollution exposures in adult Beijing residents with and without prediabetes: A panel study. Environmental Health Perspectives, 2020;128(6):067004.
https://doi.org/10.1289/EHP4906
Zhang H, Han Y, Qiu X, et al. Association of internal exposure to polycyclic aromatic hydrocarbons with inflammation and oxidative stress in prediabetic and healthy individuals. Chemosphere, 2020;253:126748.
https://doi.org/10.1016/j.chemosphere.2020.126748
Han Y, Wang Y, Li W, et al. Susceptibility of prediabetes to the health effect of air pollution: a community-based panel study with a nested case-control design. Environmental Health, 2019;18:65.
https://doi.org/10.1186/s12940-019-0502-6
Wang Y, Han Y, Zhu T, et al. A prospective study (SCOPE) comparing the cardiometabolic and respiratory effects of air pollution exposure on healthy and pre-diabetic individuals. Science China Life Science, 2018;61:46–56.
https://doi.org/10.1007/s11427-017-9074-2
